What is cellulitis? How to differentiate cellulitis from erysipelas?
Erysipelas and cellulitis are common bacterial skin infections.
Cellulitis is a spreading infection of the skin extending to the deeper tissues, involving the subcutaneous tissues (fat and soft tissue layer). Erysipelas is a specific superficial form of cellulitis, affecting the upper layers of the skin (mainly dermis with significant lymphatic involvement).
They can overlap each other, so it is not always possible to make a definite diagnosis between the two.
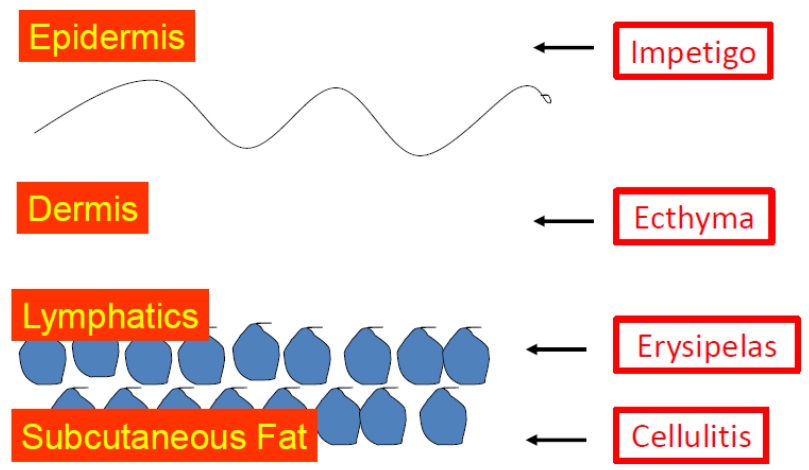 |
| Fig 1: Bacterial infections in the different layers of skin |
What causes cellulitis and erysipelas?
Germs (bacteria) are present on the skin and do not generally cause any harm (normal flora). However, if they go deep into the skin layer then they can cause infection. They generally get through a break in the skin such as cuts, wound, scratch, grazes, bites or injection or from another skin disorder like eczema, contact dermatitis, psoriasis, leg ulcer, intertrigo or tinea pedis (athlete’s foot). Our body’s immune system will try to stop the bacteria from spreading. If it fails, an infection will develop.
Both erysipelas and cellulitis are usually caused by bacteria called group A ß -haemolytic Streptococci (GABHS) and Staphylococcus aureus.
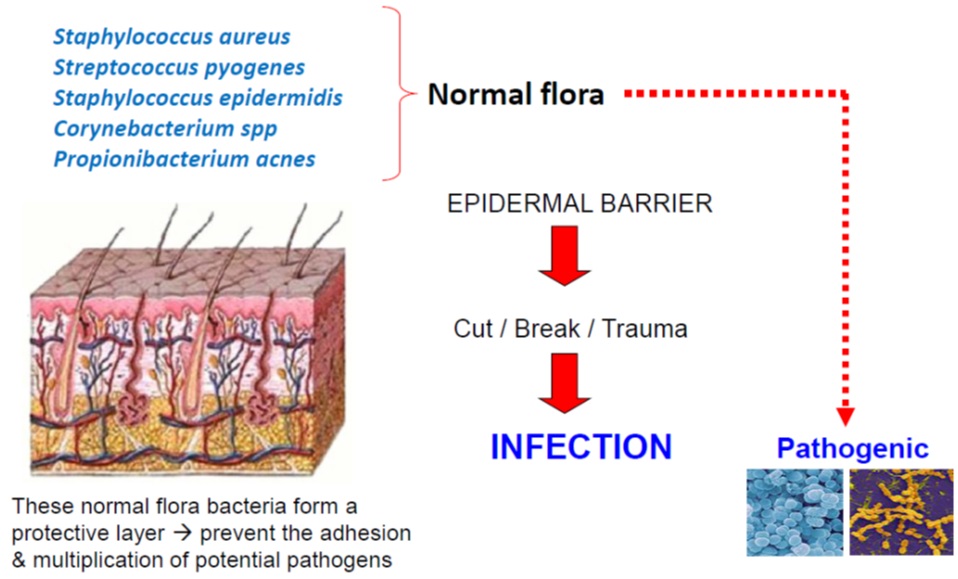 |
| Fig 2: Pathophysiology of soft tissue and skin infections (SSTIs) |
Who are at risk of getting cellulitis or erysipelas?
Anyone can get cellulitis or erysipelas. Once you’ve had it, you are more likely to get it again in the same part of the body.
There are some conditions which make cellulitis and erysipelas more likely:
- Break in the Skin Barrier
- Lacerations, bites, wounds
- Instrumentation (needles) / surgery
- Wounds (chicken pox, leg ulcer)
- Burn
- Spread from an adjacent infection (OM)
- Eczema / dermatitis
- Underlying skin diseases such as intertrigo / tinea infections (secondary infection)
- Host factors
- Poorly controlled diabetes mellitus
- Age (infant / older age)
- Impaired immune system due to illness (AIDS, cancer) or medication such as corticosteroid, chemotherapy or radiation
- Obesity
- Vascular insufficiency
- Intravenous drug use and alcoholism
What are the symptoms of cellulitis and erysipelas?
You will feel unwell with fever and shivers. The fever may start a few hours or a day before the skin changes become visible.
The affected skin (usually occurs on one side of the body) will become red, painful / sore, swollen and warm. Blisters may form in certain cases. The nearest lymph glands may become swollen and painful. The area of affected skin tends to expand over the next few hours to a few days.
Cellulitis might affect only your skin. Or it might also affect tissues underlying your skin and can spread to your lymph nodes and bloodstream. It’s important to seek immediate medical attention if cellulitis symptoms occur.
What are the signs of cellulitis and erysipelas?
Cellulitis commonly affects the lower limbs and erysipelas affects mainly on on the legs and face. However, any sites of your body can be affected.
Erysipelas typically presents as rapidly progressing fiery red, hot, thickened and painful plaque with sharp demarcation from normal surrounding skin. On the other hand, cellulitis often presents as painful, warm erythema with ill- defined edge and non-palpable borders. It is commonly preceded by systemic symptoms. It may be associated with ascending lymphangitis (red streaks on the skin above the affected area) ± regional lymphadenopathy.
Swelling and blisters may develop over the erythematous area. In severe cases, areas of skin may turn purplish or black (necrotic).
 |
 |
| Fig 3: Erysipelas | Fig 4: Cellulitis |
 |
 |
| Fig 5: Bullous Erysipelas | Fig 6: Cellulitis with ascending lymphangitis |
How to diagnose cellulitis / erysipelas?
Cellulitis and erysipelas are diagnosed clinically. A skin swab or blood tests can be taken to identify the bacteria; however identification of the bacteria is not always possible.
Is cellulitis / erysipelas serious?
The severity can range from mild to severe. This will depend on how large the affected area is, which part of the body is affected (face is more serious) and if there is any underlying medical illness.
If left untreated, the spreading infection can be life threatening.
Cellulitis and erysipelas can also lead to complications:
- Septicaemia (blood stream bacterial infection)
- Abscess (a collection of pus in the affected area)
- Infection spreading to deeper tissues, such as the muscle or bone. Necrotizing fasciitis is an example of a deep-layer infection. It represents an extreme emergency.
- Long-term swelling of the affected site due to lymphatic vessel damage
- Increased likelihood of further cellulitis or erysipelas
- Kidney damage following streptococcal infection
- Meningitis following facial erysipelas
Is cellulitis / erysipelas contagious?
No. They are different from impetigo, which is a superficial infection that can easily pass on to other people. Cellulitis / erysipelas affect the deeper layers of the skin.
Can cellulitis be cured?
Yes. Treatment with systemic antibiotics at an early stage is important to prevent the spread of infection and its related complications.
What are the treatment & prevention for cellulitis?
An oral antibiotic must be given as early as possible, and continued for 7-14 days. If the condition is not improving, higher doses and longer courses may be required. For more severe infection, they need to be hospitalized for intravenous antibiotic injections.
Most people are treated with a form of penicillin, so it is extremely important that you tell your doctor if you are allergic to penicillin.
As long as the affected area is red, swollen and hot, it should be rested and raised. The foot should be rested higher than the hip to allow gravity to reduce the swelling. Any leg swelling after the infection has resolved should be treated with compression stockings.
It is important that any breaks in the skin or concomitant skin diseases such as athlete’s foot, intertrigo or eczema, are treated to prevent repeated episodes of cellulitis. You should follow the advice on skin care to reduce breaks in the skin.
If there are repeated episodes of cellulitis, the doctor may suggest long-term prophylactic antibiotic treatment.
References
- Stevens DL et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of America. Clin Infect Dis.2014; 59(2): e10-52.
- Swartz MN. Clinical practice. Cellulitis. N Engl J Med. 2004; 350(9): 904-12.
- Gabillot-Carré M, Roujeau JC. Acute bacterial skin infections and cellulitis. Curr Opin Infect Dis. Apr 2007; 20(2):118-23.
- Thomas KS et al. Penicillin to prevent recurrent leg cellulitis. N Engl J Med. 2013;368 (18):1695-703.
| Last Reviewed | : | 23 August 2019 |
| Writer | : | Dr. Tan Wooi Chiang |
| Accreditor | : | Dr. Noor Zalmy bt. Mohd Ali Azizan |
| Reviewer | : | Dr. Nazatul Shima bt. Abd Rahim |







