A solitary pulmonary nodule (SPN) is a single abnormality in the lung that is smaller than 3 cm in diameter. It can be an incidental finding found in up to 0.2% of chest X-rays and around 1% of CT scans.
Symptom
Most persons with a SPN do not experience symptoms.
Causes
Solitary pulmonary nodules may have the following causes:
- Neoplastic (an abnormal growth that can be benign or cancerous):
- Hamartoma (an abnormal growth of normal tissues that are poorly organized)
- Inflammatory (infectious) — Granuloma (small, granular inflammatory lesions)
- Infection caused by bacteria — Tuberculosis
- Infections caused by fungi
- Hydatid cyst (a cyst formed by the larval stage of a tapeworm, Echinococcus)
- Inflammatory (non-infectious):
- Rheumatoid arthritis (a generalized disease of the connective tissues; joint pain is the main symptom)
- Wegener granulomatosis (inflammation of the small blood vessels characterized by lesions that kill the cells in different organs of the body)
- Sarcoidosis (a disease characterized by granular lesions of unknown cause that involves various organs of the body)
- Arteriovenous malformation (failure of proper or normal development of arteries and veins)
Risk Factors
The following features are important when assessing whether the SPN is benign or malignant.
- Age: Risk of malignancy increases with age.
- Risk of 3% at age 35-39 years
- Risk of 15% at age 40-49 years
- Risk of 43% at age 50-59 years
- Risk of greater than 50% in persons older than age 60
- Smoking history: A history of smoking increases the chances of the SPN being malignant.
- Prior history of cancer: People with a history of cancer in other areas of the body have a greater chance that the SPN is malignant.
- Occupational risk factors for lung cancer: Exposure to asbestos, radon, nickel, chromium, vinyl chloride, and polycyclic hydrocarbons increases the chance that the SPN is malignant.
- Travel history: People who have traveled to areas with endemic mycosis (such as histoplasmosis, coccidioidomycosis, or blastomycosis) or a high prevalence of tuberculosis have a higher chance of the SPN being benign.
- People who have a history of tuberculosis or pulmonary mycosis have a greater chance of the SPN being benign.
Investigations
- Chest radiograph: previous chest radiograph will help doctor to certain any changes of nodule character.
- CT scan thorax: The CT scan is an invaluable aid in identifying features of the nodule and determining the likelihood of cancer. In addition to the features seen on a chest X-ray, a CT scan of the chest allows better assessment of the nodule.
- Biopsy of nodule: A sample of cells is removed for examination under a microscope. Different ways are used to collect biopsy samples from the airway or lung tissue where the SPN is located. The procedures are invasive.
- Bronchoscopy: This procedure is used for SPNs that are situated closer to the walls of the airways. A bronchoscope (a thin, flexible, lighted tube with a tiny camera at the end) is inserted through the mouth or nose and down the windpipe. From there, it can be inserted into the airways (bronchi) of the lungs. During bronchoscopy, the health care professional takes a biopsy sample from the SPN. If the lesion is not easily accessible on the airway wall or is smaller than 2 cm in diameter, a needle biopsy may be performed. This procedure is called a trans-bronchial needle aspiration (TBNA) biopsy.
- Transthoracic needle aspiration (TTNA) biopsy: This type of biopsy is used if the lesion is not easily accessible on the airway wall or is smaller than 2 cm in diameter. If the SPN is on the periphery of the lung, a biopsy sample has to be taken with the help of a needle inserted through the chest wall and into the SPN. It is usually performed with CT/ultrasound guidance. With SPNs larger than 2 cm in diameter, the diagnostic accuracy is higher (90%-95%). However, the accuracy decreases (60%-80%) in nodules that are smaller than 2 cm in diameter.
- Video-assisted thoracoscopy (VATS) is performed with the help of a thoracoscope (a flexible, lighted tube with a tiny camera at the end) inserted into the chest through a small cut on the chest wall. The camera displays the image on a TV screen, and the surgeon uses the display to guide the operation. This is an option that may be used to remove the nodule for both treatment and for confirming diagnosis.
| Solitary pulmonary nodule |
|---|
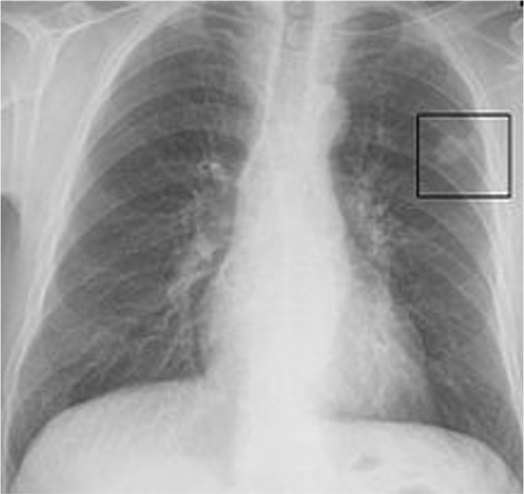 |
| Chest X-ray showing a solitary pulmonary nodule (indicated by a black box) in the left upper lobe. |
Treatment
| Patient categories | Follow up plan |
|---|---|
|
Persons with benign SPN: Determining that the SPN is benign is based on the following:
|
Persons who have been diagnosed with benign SPN should undergo chest X-ray or CT scans every three to four months in the first year, every six months in the second year, and once every year for up to five years. |
|
Persons with a malignant SPN |
Persons who have been diagnosed with a malignant SPN based on the results of the exams and tests should have the nodule surgically removed. |
|
Persons with SPN that cannot be classified as either benign or malignant |
However, as many as 75% of these patients have malignant nodules on further evaluation. Therefore, such persons are also advised to have it surgically removed. |
| Last Reviewed | : | 13 June 2017 |
| Writer/Translator | : | Dr. Kasuma bt. Mohamed Nordin |
| Accreditor | : | Dr. Nurhayati bt. Mohd Marzuki |







